
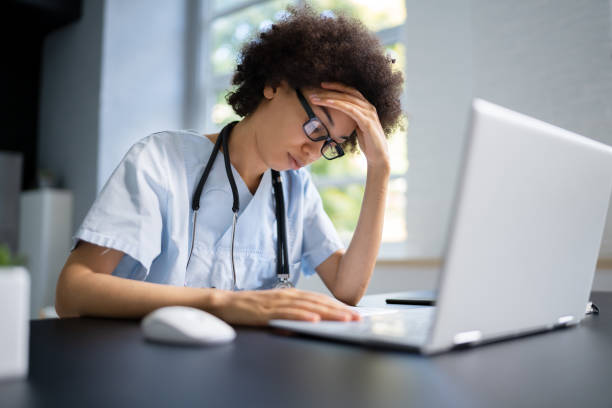
Most behavioral and mental health procedures require providers to obtain prior authorization before treatment. Navigating the challenges of mental health billing means tackling the complexities of insurance policies and their impact on financial workflows. It’s essential to verify eligibility and benefits checks to avoid claim issues and ensure providers understand patient benefits before delivering services. CMS advises including detailed documentation, such as timesheets, encounter notes, specifics, and proof that the care team developed the treatment plan collaboratively with the patient and their family. These factors make the process demanding, but as a top mental health billing company, we can assist with:
Mon – Fri
08.00 -18.00
Sat – Sun
09.00 -15.00
Most behavioral and mental health procedures require providers to obtain prior authorization before treatment. Navigating the challenges of mental health billing means tackling the complexities of insurance policies and their impact on financial workflows. It's essential to verify eligibility and benefits checks to avoid claim issues and ensure providers understand patient benefits before delivering services. CMS advises including detailed documentation, such as timesheets, encounter notes, specifics, and proof that the care team developed the treatment plan collaboratively with the patient and their family. These factors make the process demanding, but as a top mental health billing company, we can assist with:



8655 Bay Parkway, Brooklyn NY 11214
Mon To Friday
9:00 am to 5: 00 pm
Contact us : +1 862 413 4315
Stay in the know with news and promotions